| Kaiser Health News Posted: 15 Apr 2022 02:30 AM PDT
| It’s Not Just Doctors and Nurses. Veterinarians Are Burning Out, Too. Posted: 15 Apr 2022 02:00 AM PDT If you or someone you know is considering suicide, please call the National Suicide Prevention Lifeline: 1-800-273-TALK (8255). At the park near Duboce Triangle in San Francisco, 5 p.m. is canine happy hour. About 40 dogs run around, chasing balls and wrestling, as their owners coo and ’90s hip-hop bumps out of a portable speaker. One recent afternoon, a Chihuahua mix named Honey lounged on a bench wearing a blue tutu and a string of pearls. Her owner, Diana McAllister, fed her homemade treats from a zip-close bag, then popped one into her own mouth. After spending two years at home through the pandemic, it’s clear that for a lot of these owners, their dogs are their children. “I always say, dogs are people, so I love him,” said Yves Dudley, looking on as her 9-month-old collie-schnauzer mix played in the grass. Across the country, about 23 million families adopted a pet in the first year of the pandemic. Other pet owners, working from home, started paying more attention to their animals’ daily routines, noticing symptoms like vomiting or coughing. The resulting spike in pet health concerns has been straining a corner of the medical world that doesn’t get as much attention as doctors and nurses: veterinarians. The overwork and staffing shortages of the pandemic have affected veterinarians as much as other doctors and nurses, and dealing with the constant moral dilemmas and emotional output was driving many to burn out even before 2020. The mean salary for vets is about $110,000 per year, according to the Bureau of Labor Statistics, about half that of physicians catering to people. At the Society for the Prevention of Cruelty to Animals’ veterinary hospital in San Francisco, so many vets and technicians have left that the clinic has had to cut back its hours, said veterinarian Kathy Gervais. Dog owners say they’ve had to wait months for vet appointments or drive to vets far from home to get care. “Getting your dog in to see the vet is as competitive as trying to buy Coachella tickets online,” said Laura Vittet, whose golden retriever, Gertrude, is 1½ years old. “You have to wait by the phone, you have to be ready to refresh your browser. It’s a very intense experience.” Gervais said she works 12-hour days, constantly zigzagging from new puppies to dying cats. And the whole time, she takes care of their humans, too. “To these people, and especially in these times, this is their love,” she said, thinking especially of the owners who dress and coif and cook for their dogs. “This is their being, this is what they live for. And for vets, it’s very hard for us to draw the line.” 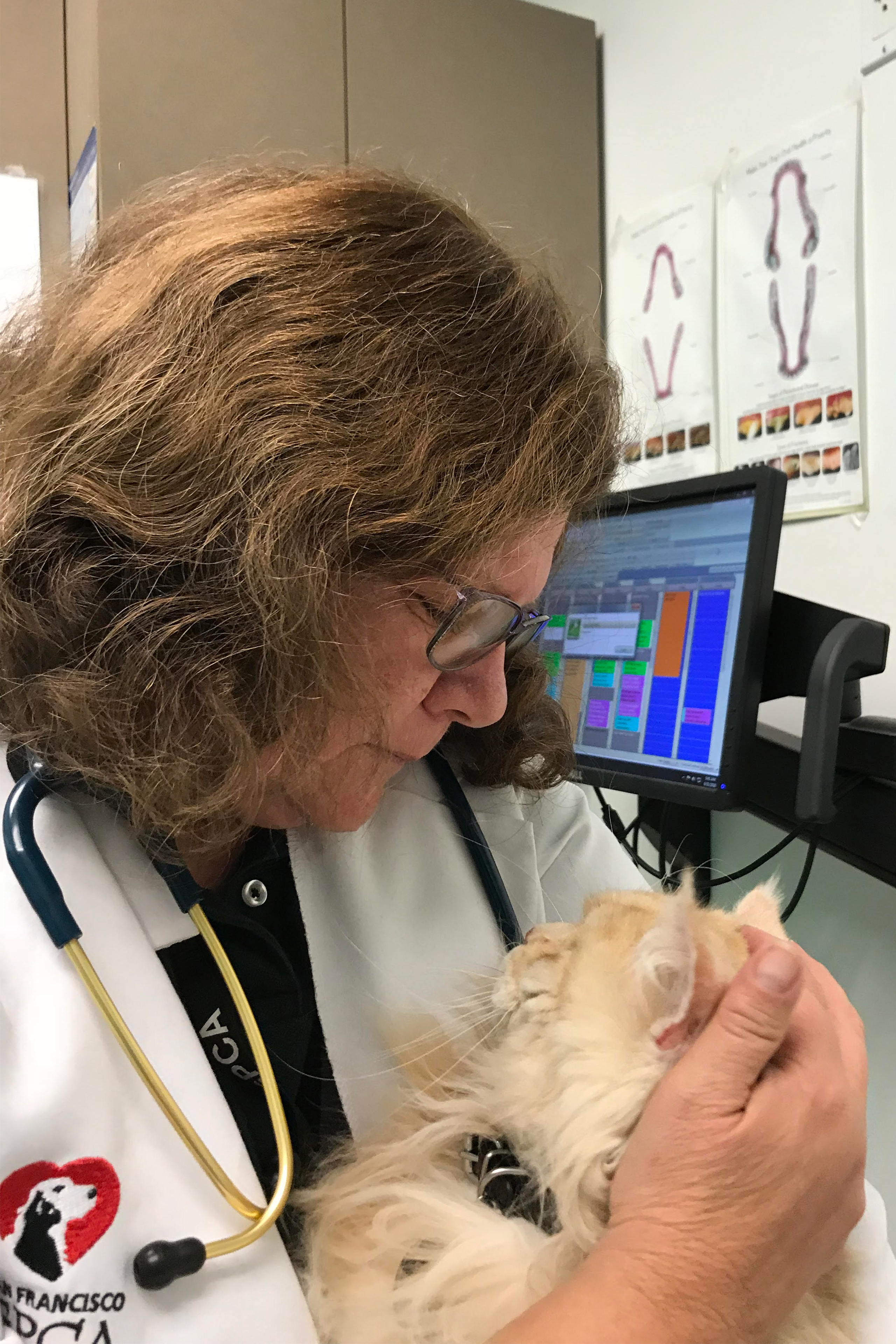 Empathy overload and compassion fatigue affect veterinarians’ mental health. They carry the weight of having to euthanize animals that could be saved but whose owners can’t afford the care. Gervais said her practice euthanizes about five animals every day. Some upset owners become downright abusive when a pet is in distress, berating vets or later bullying them online. “I dare you to try to talk to a veterinarian who’s been in practice more than five years who doesn’t know somebody who has committed suicide,” said Gervais. “I, unfortunately, can count on more than 10 fingers: classmates, colleagues, people I’ve dated.” One in 6 veterinarians have considered suicide, according to studies from the Centers for Disease Control and Prevention. While male vets are 1.6 times as likely to die by suicide as the general population, female vets are 2.4 times as likely, and 80% of vets are women. In the early months of the pandemic, Gervais could see things getting worse. She helped organize the Veterinary Mental Health Initiative, which offers free support groups and one-on-one help to vets across the country. All the facilitators have doctorate-level training, said founder and director Katie Lawlor, also a psychologist, and they’re all familiar with the issues troubling vets. “Burnout, compassion fatigue, managing panic attacks, how to communicate with both supervisors, colleagues, and clients when you’re under extreme deadlines or very intense stress,” she said. “And the loss of their own companion animals.” The initiative helped Dr. Razyeeh Mazaheri work through the anxiety she was feeling every day caring for animals at a clinic outside Chicago last year. The clinic was regularly double- or triple-booked. As a new vet — Mazaheri graduated from veterinary school last spring — juggling so many cases was terrifying. “I just feel like if I make a mistake, that is a problem. And if I make a mistake and kill something, that is my fault,” she said, tearing up. “I just knew that I was burned out.” Through the support groups, Mazaheri was able to see that others shared her concerns and she learned coping tools. The initiative, housed under the nonprofit Shanti Project, has groups specifically for emergency vets, vet technicians, recent grads like Mazaheri, and longtime vets like Kathy Gervais who have more than 20 or 30 years of experience.  “I’ve had people look at me sometimes when they’ve seen me really tired, going, 'Kathy, walk away,’” she said. “I’m not ready to do it because, bottom line, I love my job. It is a vocation. It is a passion. And it’s hard to walk away from that,” she said. “But if it’s going to kill me on the flip side, I would hope I could just say, 'OK, that’s it. I’m done.’” This story is part of a partnership that includes KQED, NPR and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | Readers and Tweeters Sound Alarm Over Nurse’s Homicide Trial Posted: 15 Apr 2022 02:00 AM PDT Letters to the Editor is a periodic feature. We welcome all comments and will publish a selection. We edit for length and clarity and require full names. Nursing on Trial It’s about time that nurses are held accountable for their jobs (“As a Nurse Faces Prison for a Deadly Error, Her Colleagues Worry: Could I Be Next?” March 22). Several measures, training, and computer systems are already in place to try to ensure that nurses do not make medication errors. But they just ignore them or manually override the computer. Medication errors were rampant at my last hospital job. Every hospital has an anonymous system where any employee can report these kinds of errors. I reported several medication errors, and nothing was ever done about it. No meetings, no emails, no “here is an example and we need to do better.” So I gave up reporting them on the system. A few days before I retired, I was telling the night nurse about a med error I prevented on a new patient admitted the night before. Turns out she was the one who made the error! Her response was, “Shouldn’t pharmacy have caught that?” She took no responsibility for not clarifying the order. And she had been a nurse for over two decades. And the med error was close to an overdose amount, according to the pharmacy. My experience was that there is very little accountability in nursing unless a manager doesn’t like you. It has nothing to do with the ability to do the job or patient safety. — Phyllis Mitchell, Laguna Woods, California This case will have far reaching implications. This is what happens when we automate everything and don't think about the implications. https://t.co/sIMftvc4jt @annlcutrell @JohnMaynardCPA — Tom Wriggins (@TomWriggins) March 23, 2022
— Tom Wriggins, Naples, Florida I’ve been a registered nurse for two years and was a licensed practical nurse for 10 years. What RaDonda Vaught did is abysmally wrong on so many levels. I cannot believe the number of licensed professionals trying to defend pure malpractice and negligence (“Reaction to the RaDonda Vaught Verdict: KHN Wants to Hear From Nurses,” March 30). This is not a “system problem,” it’s a RaDonda problem. You’re telling me she should be exonerated after blowing past 10 huge red flags?! They said “Stop what you’re doing and make sure it’s correct. This is a PARALYTIC drug.” No more system checks would have made a difference because she ignored every single one that came up. Medical professionals rely way too much on technology. Blaming technology and “the system” are poor excuses for what happened. If I was drinking, then decided to drive my car at 80 mph through a neighborhood, blast through stop signs and red lights and kill a child, should I be forgiven with a slap on the wrist? Pure and simple negligence. These people trying to defend Vaught are all about professional responsibility, and want RNs to be respected, but think this is OK? The RN is a professional, licensed nurse and is the bottom line against errors that slip through the system. If she would have taken two seconds to think about the five rights, this never would have happened, regardless of whether there were problems with the automated medication-dispensing system. This is basic Nursing 101. This case really upsets me. The fact nurses are trying to shift blame away from her is alarming. And if they’re worried it could happen to them, then maybe they shouldn’t be practicing. — Paul Dziejman, Depew, New York this trial that resulted in the criminalization of medical errors also revealed systemic issues in the hospital setting. if unaddressed, the precedence of this ruling will have negative impacts on the nursing profession. #RaDondaVaught #PM760https://t.co/KKFOyEPtKv — Katie Wee (@wee_insun) March 29, 2022
— Katie Wee, Boston One important cause of potential nursing errors not mentioned in the article is understaffing. My RN sister’s intensive care unit expects as many as six nurses gone soon, from her shift alone. And the worse conditions are, the less likely even agency nurses will accept a position. Do dedicated RNs stay for the patients’ sake, or leave to protect themselves? You can help both patients and nurses by supporting safe staffing legislation in your state. — Gloria Kohut, Grand Rapids, Michigan "THIS COULD BE ME" Heartbreaking case of automated dispensing cabinet (ADC) override gone wrong https://t.co/DtZ1WA258U#medsafety #medicationerror #medicationsafety #secondvictim #ilovemedsafety #nurses #hospitals — Sunny Ro (@SunnyRoPharmD) March 22, 2022
— Sunny Ro, Philadelphia The Fallout of Prosecuting Medical Errors In the article “Nurse Convicted of Neglect and Negligent Homicide for Fatal Drug Error” (March 25), I found myself reflecting on my future nursing career. Although it is clear RaDonda Vaught was guilty of a medication error that led to the death of a patient, I can sympathize. The hateful public ridicule she has been given and the defaming comments from the prosecutors regarding her nursing character being “uncaring … and abandoning her patient” are alarming. It creates an alternative narrative of what has taken place, and that is that Vaught intentionally harmed a patient, not accidentally. Reporting any type of medical error whether it is small or large is crucial in identifying safety issues in nursing care and, with the handling of the Vaught case, some nurses may feel that admitting to a mistake can cost them their job and/or their life. To build progress toward improving health care delivery, the handling of medical errors should be judged fairly, and without shaming nurses who have dedicated their lives to protecting and healing patients. As stated in the article, “Health care just changed forever,” and this creates an environment of fear and mistrust, and an unsupportive system for nurses to come. — Katarina Velardez, San Francisco Be frightened. For those of you involved in making medical care safer and more reliable, a recent prosecution of a nurse for a medical error may set our efforts for "Just Culture" back a few decades. We learn, not blame. @AAPneonatal @D8Neonatal https://t.co/NpWqS5gfBh — james barry (@skideepowder) April 1, 2022
— James Barry, Denver I am saddened that with all the efforts made to advance patient safety that RaDonda Vaught was prosecuted versus Vanderbilt University Medical Center and/or the drug-dispensing vendor. We know that medication errors occur every day and we need to continuously work to reengineer things to make it hard to make an error. Having been a nurse for many years, I am appalled at the manipulation of calling nurses who work in challenging conditions heroes until something goes wrong. This error was completely understandable and predictable. First of all, after decades, why are these systems still not programmed to recognize both generic and brand names? That alone would have prevented this medication error. Secondly, as with all broken systems, when there were known dispensing issues with the drug-dispensing system, why wasn’t Vanderbilt proactive? If nurses needed to override the system routinely, why didn’t a patient-safety expert conduct an FMEA (failure mode event analysis) and remove all high-risk drugs from the drug-dispensing machine? Vanderbilt has failed patients and nurses and should step up. Without focusing on investigating what went wrong and sharing the findings with other organizations, health care cannot learn. Vendors for these systems are also failing patients and nurses. Shouldn’t there be requirements by now for all searches on these systems to include both brand and generic drug names? We have created a distraction with this trial to mistakenly help Americans feel safe. We removed this “bad” nurse, so we are safe now. The truth is patients are now less safe than before this verdict. Nurses always live in fear of making a mistake and causing harm. We struggle to continue to work in environments where our voices for patient safety are not heard and are silenced. This is a step backward for all of American health care in which medication errors remain the No. 1 type of error. We have neglected to be transparent and learn how to prevent another nurse from making the same mistake. This has reaffirmed for me and other nurses that you will be asked to work yourself to exhaustion, give all your mental and physical strength and be called a hero so long as it benefits an organization or society, but when something goes wrong you will be unsympathetically discarded and made a villain. How sad. — Carole Cassidy, Newtown Square, Pennsylvania She made a critical mistake, but is she deserving of serving time in prison? Nurse Convicted of Neglect and Negligent Homicide for Fatal Drug Error https://t.co/8DjvYVrolr via @khnews — Garry Klein (@GarryfromIowa) April 6, 2022
— Garry Klein, Iowa City, Iowa A Family Caregiver’s Plea Another essential part of family caregivers should be a requirement for medical records to be able to be accessed by the family (“To Families’ Dismay, Biden Nursing Home Reform Doesn’t View Them as Essential Caregivers,” March 22). I am the legal guardian of my sister-in-law and have no access to her medical records. She is not capable of answering my questions accurately. I need to be able to see those records to monitor her medications and follow what care is being provided. It isn’t as if they don’t use computers. It would require no extra work on the staff’s part. And we should have also access to the same info the staff sees. Because I have no access to her records, it made no sense for me to continue to take her to her own doctor or psychiatrist because I can no longer answer the questions they ask about her activity and her health and eating. I visit twice a week and do some of the little things that the staff misses. There are times I suspect a missed dose of medication or a medication change, but there is no way to know for sure. I am considering moving her to a different facility for this reason. I just think this is a vital part of including family, especially if they have guardianship. — Theresa Smith, St. Joseph, Missouri Really? There is nothing "informal" about family caregiving. Family/close friends are the most trusted allies & care coordinators for residents of LTC facilities. They are essential to the well-being of vulnerable older adults. https://t.co/TI60SRGrmR via @khnews — Lynn Friss Feinberg (@FeinbergLynn) March 22, 2022
— Lynn Friss Feinberg, Washington, D.C. Concerns About an Autism Therapy I’m concerned about the article “Delays for Autism Diagnosis and Treatment Grew Even Longer During the Pandemic” (March 30) because it does not include any input from an actually autistic adult and it supports ABA [applied behavioral analysis] therapy as the gold standard for autism treatment, a theory dethroned by several recent studies. I was recently diagnosed as autistic as an adult and have done thousands of hours of research on what is the best treatment for myself and an underage family member under my care. ABA is extremely expensive and time-consuming and not proved effective, according to a recent study by the Department of Defense, and could be actively harmful to children receiving the therapy. In addition, the therapy practice is ethically questionable, as it was founded by Ole Ivar Lovaas — yes, the same guy who founded gay conversion therapy. And forcing an autistic kid to “convert” to looking “normal” is equally harmful. Therapies that should be recommended for recently diagnosed children should be occupational therapy, to determine sensory issues and a sensory routine to support those needs; speech therapy (if needed); and training in the collaborative problem-solving method by Dr. Ross Greene. For more expert knowledge than mine on the harms of ABA, see the work of the Therapist Neurodiversity Collective. Thank you for your attention. — Andrea Hebert, Nashville, Tennessee You know whats more heartbreaking for parents who have children with autism? Nothing will be done to help them at all. They were abandoned, and CNN article is a fake concern considering they incited lockdowns and covid hysteria.https://t.co/QcgoA9rZhA — Ndee -Jkid- Okeh (@Jkid4) March 29, 2022
— Ndubuisi Okeh, Capitol Heights, Maryland More on Vaccines and Covid Transmission As one of your readers, I value your overall mission. I am writing with concern about the article by Aaron Bolton, called “Patients With Vulnerable Immune Systems Worry Vaccine Exemptions May Put Them in Peril” (March 22). The premise of the article is that unvaccinated health care workers are putting patients at risk, ignoring the widely acknowledged fact that vaccination does not prevent, or even reduce, transmission. I would expect greater diligence in demanding objectivity from your featured authors, rather than perpetuating fear-based claims that unfairly target those front-line workers who have been working overtime for the health of the public. This article offers information on the transmission of covid-19 that may help inform which pieces you choose to run in the future. — Hannah Miller, Missoula, Montana Peek into the danger for the #immunecompromised. Lots of fake religious & medical exemption forms out there. Wonder why we are so paranoid. #PandemicoftheUnvaccinated https://t.co/cCJi6X7gFI — Barbara Katz-Chobert (@KatzChobert) March 24, 2022
— Barbara Katz-Chobert, Philadelphia Removing the Stigma of Miscarriage I am a student nurse at California State University-East Bay and am writing regarding the article “After Miscarriages, Workers Have Few Guarantees for Time off or Job-Based Help” (Jan. 26). I would like to start off by simply saying thank you. You discussed a topic that has gone ignored for so long. It is disheartening to read that not even half of our country has enacted laws that provide paid sick leave for miscarriages. My hope is that articles like yours will allow us to have deeper, meaningful, and destigmatized discussions about miscarriages — and, more so, to acknowledge the emotional, mental, and physical impact on anyone who may have experienced such loss. — Catherine Zelidon-Sarcos, Pittsburg, California Excellent essay on how we can honor women in the workplace. If we want more kids, then we have to value women at work.After Miscarriages, Workers Have Few Guarantees for Time Off or Job-Based Help | Kaiser Health News https://t.co/5oaNdqqAFR — dacortright🇺🇦 (@david_cort7) March 22, 2022
— David Cortright, Austin, Texas Countering the 'Abortifacients’ Argument The morning-after pill and IUDs work by preventing conception, not by preventing implantation (HealthBent: “As Red States Push Strident Abortion Bans, Other Restrictions Suddenly Look Less Extreme,” March 30). The hormonal IUDs create a mucus plug that prevents the passage of sperm. Copper IUDs create a sterile inflammatory reaction that essentially neutralizes the ability of the sperm to penetrate the egg. Emergency contraception pills prevent ovulation. By perpetuating the anti-choice narrative that these methods work by preventing implantation, you are discouraging and stigmatizing their use. — Amy O’Meara, Kamuela, Hawaii You cannot completely ban abortion, because the far-right can’t even agree on what an abortion is. 18 weeks, 6 weeks, conception, birth control, masturbation, IVF. Every new restriction opens the door to an even more draconian law. https://t.co/0BUiRIC9xQ — Trojan Horse News (@realTHNews) March 30, 2022
— Kate Woods, Atlanta The Cost of Treating Troubled Kids The $400-plus-a-day average reimbursement per child equates to almost $148,000 a year. That seems like plenty to accommodate one of these children (“Montana Is Sending Troubled Kids to Out-of-State Programs That Have Been Accused of Abuse,” March 25). I also think the story glosses over the challenges that these children present to the schools. — Mike Morgan, Bozeman, Montana Education policy is health policy. Working in a public high school, this is an appalling action by the state of Montana. #pm760https://t.co/3UyH7JhdvB — Ian O'Neil (@IanONeil12) March 25, 2022
— Ian O’Neil, Boston Before you write an article about out-of-state abuse and quote someone … “Shipping those kids out of state for treatment for behavioral and substance use disorders comes with a high price tag, and often the children’s issues are not resolved or are even worse, said Michael Chavers, CEO of Yellowstone Boys and Girls Ranch. 'When they return to us, they return with worse outcomes and for higher cost,’ Chavers told Montana lawmakers last fall.” … you might want to look at the background of the Yellowstone Boys and Girls Ranch, as it had to pay out $300,000 in a boy’s sexual abuse case in 2018. Let’s clean up our backyard first. Do some research before throwing stones. The author of the article should have done better research on the business or people they were using as “experts.” Shame on YBGR and Chavers for making comments as if they are without problems. — Kim Hover, Stevensville, Montana Embracing Personalized Medicine In the article “Big Pharma Is Betting on Bigger Political Ambitions From Sen. Tim Scott” (March 28), KHN describes the Personalized Medicine Coalition and its work inaccurately for a second time (see also “A Senator From Arizona Emerges As a Pharma Favorite,” May 29, 2020). PMC, a 501(c)(3) nonprofit organization comprising 14 distinct stakeholder groups within health care, with the largest segment made up of “research, education, and clinical care institutions,” is not a trade association and does not represent any single industry or business model. Moreover, your implication that personalized or precision medicine jacks up the costs of pharmaceutical products misses the mark. Its goal, in addition to promising better outcomes for patients, is to lower systemic costs for health care by making it more efficient. Personalized medicine has been shown to save health systems money while improving patient care. The Teachers’ Retirement System of the state of Kentucky, for example, has found that integrating genetic testing into prescribing decisions saved the system $5,176 per enrolled member by targeting treatments to only those patients who will benefit, sparing expenses and side effects for those who will not. For cancer patients, Intermountain Healthcare has also found that genomic testing can lengthen progression-free survival rates without increasing costs. Sen. Scott may or may not have his eye on higher office, but he is correct that we could do a lot worse than embrace personalized medicine. — Edward Abrahams, president of the Personalized Medicine Coalition, Washington, D.C. The Long Arm of Big Pharma I just learned about your website, thanks to a recent daily current events analysis done by American history professor Heather Cox Richardson, which cited a link to the amazing webpage providing insight into Big Pharma’s deep-pocket reach into Congress. I have nothing but admiration and appreciation for the work that went into making such a page. And I say that despite the unfortunate personal surprise and bummer it was to see my congressman listed prominently as the “Freshman Favorite,” Rep. Frank J. Mrvan. Living here in Indiana means Eli Lilly has always had an outsize influence on societal affairs. So the fact that it is at the very top of his list of pharma donors is not surprising. But then there were all the other pharma companies underneath Eli Lilly — an eyebrow-soaring number, actually. Because the dates go back to 2007, I had been hoping to compare his reputation against his predecessor for this district, Pete Visclosky. The man was highly esteemed and as such remained incumbent here since I can remember, at least since I was in high school in 2000. I hope your project can fill in data on predecessor representatives. It would help folks like me contextualize just how much pharma donations may have already been a problem. The underlying reality is that each individual receiving donations does so on behalf of a particular office — therefore, my interests as a citizen are aggressively bought out. I’d like to know if my say with my previous congressional representative was diluted at all. Particularly when it comes to certain personal aspects of the pharmaceutical industry, like the $16,000-a-month medication that kept my mother alive for a while longer in her years-long fight against cancer, which she maintained until one day she couldn’t anymore. (Without the Affordable Care Act’s insurance having “arrived in time” for her finding a lump and being diagnosed, our ability to afford such a treatment would have been nonexistent.) In other words: I would very much appreciate the possibility to know how angry and resentful, and therefore politically active, I should be when it comes to the donation-driven influence pharma has had on this small bit of democracy assigned to me, my family, my friends, and my home community by and large. Thanks again for the outstanding work. It is very, very appreciated! — Tomas Feher, Chesterton, Indiana Babies Die as Congenital #Syphilis Continues a Decade-Long Surge Across the #US. Highest rates are in Southern US (#NewMexico, #Texas, #Oklahoma #California) https://t.co/perolRHKf6 via @CalHealthline — George Monks, M.D. (@GeorgeMonks11) April 13, 2022
— Dr. George Monks, Tulsa, Oklahoma Combating Congenital Syphilis It’s heartbreaking, yet unsurprising, that the rates of congenital syphilis are increasing in the U.S. (“Babies Die as Congenital Syphilis Continues a Decade-Long Surge Across the US,” April 12). Public health departments are underfunded and reproductive rights have been under attack for many years, especially since Donald Trump’s presidency. The defunding of clinics, like Planned Parenthood, due to anti-abortion legislation across the country, also means that many people seeking STD screening and treatment are losing places to do so. As a birth worker in Los Angeles, I witnessed firsthand how lack of access to health care impacts communities of color through structural racism. It is unacceptable that babies are dying from a totally treatable illness, due to a lack of staff and resources to help pregnant people with syphilis receive the diagnosis and treatment they need. Just as we had to get creative during the pandemic, this health problem requires creative solutions, partnership, and technology. How great would it be if a patient could receive their STD results and directories of places to pick up medications to get treatment, just as they can with covid-19. A solution must be found quickly. The health and well-being of babies, especially babies of color who are being affected at higher rates, depends on it. — Candy Ramirez-Hale, Oakland, California KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | KHN’s ‘What the Health?’: News You Might Have Missed Posted: 14 Apr 2022 12:40 PM PDT Can’t see the audio player? Click here to listen on Acast. You can also listen on Spotify, Apple Podcasts, Stitcher, Pocket Casts or wherever you listen to podcasts. It’s been extra busy on the health policy beat lately, so a congressional recess provides a chance to explore some of the important stories that people might have missed, like Medicare’s decision to dramatically limit coverage of Aduhelm, the controversial new drug to treat Alzheimer’s disease. And even with Congress out, states are rushing to either restrict or expand access to abortion, ahead of a key Supreme Court ruling expected later this spring or summer. This week’s panelists are Julie Rovner of KHN, Margot Sanger-Katz of The New York Times, Joanne Kenen of Politico and the Johns Hopkins Bloomberg School of Public Health, and Alice Miranda Ollstein of Politico. Among the takeaways from this week’s episode: - The decision by the Centers for Medicare & Medicaid Services to limit Medicare’s coverage of Aduhelm only to beneficiaries who also enroll in clinical studies of the new Alzheimer’s drug came despite intense pressure from patients and advocacy groups who are frustrated by the lack of new therapies for this devastating disease. But the federal agency also appears to have been swayed by arguments by some researchers and public health experts that the earlier research on the drug was faulty.
- The dust-up over Medicare coverage for Aduhelm points to a source of tension in the U.S. health system: Different government agencies have overlapping authorities. This dispute is between the FDA, which approved the drug despite serious questions about its effectiveness and safety, and CMS, which had to decide whether to cover the cost of a very controversial drug that is also very expensive. But similar tensions also have played out between the FDA and the Centers for Disease Control and Prevention over covid-19 vaccine schedules and eligibility.
- A recent Bloomberg report looked at concerns that the federal government is overpaying for beneficiaries enrolled in private Medicare Advantage plans. More progressive Democratic members of Congress have long complained about this, but Republicans are strong supporters of the Medicare Advantage program.
- Despite the complaints of some on the left about the excess funding of these Medicare plans, they have been growing. That is, in part, because the traditional Medicare program has many holes and cost-sharing responsibilities that people with modest incomes are nervous about shouldering, and Medicare Advantage has become attractive to them. That has complicated the formerly partisan politics over the program.
- The Biden administration is reportedly in discussions with several states about setting up programs to import cheaper drugs from Canada. For the Democrats, this could be a strong campaign talking point — much like efforts on Capitol Hill to cap the price of insulin — about trying to help people with a serious pocketbook issue. Drug prices have consistently been a consumer concern.
- However, it’s not clear whether Canada is interested in helping the U.S. with a drug import program and, even if it did, there’s no indication that the amount of drugs Canadians could provide would significantly influence prices in this country.
- Oklahoma’s governor has signed a bill that would make it a felony to perform an abortion, and Florida’s governor on Thursday approved a bill moving the limit for an abortion from 24 weeks to 15 weeks. As the country waits for the Supreme Court to rule on a case this summer that could overturn or weaken the landmark Roe v. Wade decision, conservative states are racing to find ways to limit or ban abortions.
- If the Supreme Court does upend protections guaranteed under the Roe decision, it is unlikely that clinics in states that are preserving the right to an abortion will be able to fill the need.
- Yet even with the growing movement in conservative states, abortion-rights supporters were stunned this week when a Texas prosecutor filed murder charges against a woman who had an abortion. The charges, however, were quickly dismissed.
- The CDC this week released new data showing a rise in 2020 in the number of cases of gonorrhea and syphilis — likely the byproduct of less access to health care during the early stages of the pandemic. Although the diseases can easily be cured with antibiotics, the public may not realize the need to seek medical care or the devastating consequences of letting the diseases go untreated.
- The CDC also reported that drug overdose deaths reached a record high last year.
Plus, for extra credit, the panelists recommend their favorite health policy stories of the week they think you should read, too: Julie Rovner: Politico’s “Mice Occupy FDA Offices After Food Left Behind in Pandemic,” by David Lim and Lauren Gardner Margot Sanger-Katz: Health Affairs’ “Many Medicare Beneficiaries Do Not Fill High-Price Specialty Drug Prescriptions,” by Stacie B. Dusetzina et. al Joanne Kenen: Vox’s “America Needs More Doctors and Nurses to Survive the Next Pandemic,” by Dylan Scott Alice Miranda Ollstein: Politico’s “Republicans See CDC’s Policy Change as 'Massive Political Loser for Democrats,’” by Alice Miranda Ollstein and Krista Mahr Also discussed on this week’s podcast: Bloomberg’s “Major Insurers Are Scamming Billions From Medicare, Whistle-Blowers Say,” by John Tozzi KHN’s “Researcher: Medicare Advantage Plans Costing Billions More Than They Should,” by Fred Schulte KHN’s “'What the Health?’: The Drug Price Dilemma,” featuring Stacie B. Dusetzina To hear all our podcasts, click here. And subscribe to KHN’s What the Health? on Spotify, Apple Podcasts, Stitcher, Pocket Casts or wherever you listen to podcasts. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | How a Former Catholic Priest Is Navigating a California Medicaid Plan Through Big Changes Posted: 14 Apr 2022 02:00 AM PDT ORANGE, Calif. — For Michael Hunn, the path from priesthood to health care was seamless. Hunn, a native of St. Louis, counseled hospitalized patients as a Catholic priest in the 1980s before leaving the clergy and shifting to health care administration. Over the next three decades, he was CEO of nine different hospitals — in California, Texas, and Missouri — among other senior executive positions. Across his unusual trajectory, there’s been a common thread: a desire to help people. “It was always in me to want to do that,” said Hunn, 66, who remains a devout Catholic. He asked the church to release him from clerical duties when he decided to pursue a lay life and the opportunity to marry. In March, Hunn was formally named CEO of CalOptima, the publicly run health insurance plan for Orange County’s Medi-Cal enrollees. Medi-Cal is California’s version of Medicaid, the federal-state program that provides health coverage to people with low incomes. Hunn stepped in late last year as CalOptima’s interim CEO after the previous chief executive, Richard Sanchez, retired. Board members praised Hunn’s leadership and said his decades of health care experience made him the right person to guide the agency through massive changes coming to Medi-Cal. CalOptima, one of the state’s largest Medi-Cal plans, serves 882,000 members — over a quarter of Orange County’s population. Many enrollees need help with housing and employment, in addition to medical and mental health care. CalOptima, like all other Medi-Cal plans, has committed to participating in a new initiative, California Advancing and Innovating Medi-Cal, or CalAIM. The $6 billion experiment is intended to provide vulnerable enrollees with nontraditional services — such as housing and food assistance, detoxification, and home modifications — that can improve their health. Hunn, who studied health care ethics as a seminary student and frequently consulted on end-of-life decisions while making hospital rounds as a priest, said he’s using CalAIM to provide CalOptima members with housing assistance and recuperative care, which gives patients — some of them homeless — a respite after they’re discharged from the hospital. More services could be added later. Meanwhile, the state is seeking greater oversight of all Medi-Cal health plans, which could put pressure on Hunn. The California Department of Health Care Services, which runs Medi-Cal, is working up new health plan contracts that will increase regulations and establish stricter reporting requirements starting in 2024. And CalOptima could face competition for the first time if the state allows Kaiser Permanente to jump into the fray as planned. There are times when Hunn’s duties at CalOptima conflict with his religious creed. Medi-Cal pays for reproductive care, such as abortions, that is banned by Catholic health doctrine. And it covers doctor visits and lethal drugs for terminally ill patients who choose to end their lives, an act the Vatican has called “intrinsically evil.” KHN reporter Bernard J. Wolfson sat down with Hunn in his office on the ninth floor of CalOptima’s headquarters to talk about his transformation from priest to health care executive and the changes in Medi-Cal. The interview has been edited for length and clarity. Q: Did you ever consider a more hands-on role in health care — becoming a doctor, for example? Before I went into the theologate, I did pick up an application for Saint Louis University medical school. I seriously thought maybe I should pursue medicine, because I loved it so much having worked in the hospitals. I prayed about it. I talked to my mother, primarily, about it. She said, “Follow your heart. Do what you think is right for you, but I think the church is calling you.” Q: How do you reconcile your Catholic faith with running an organization that pays for reproductive and end-of-life care? I am not a moral arbiter for another’s decision, so I set that aside and leave what I believe at home. On the professional side, I will fulfill the responsibility and duty as required. Q: The Kaiser Permanente deal with the state, if approved, would take patients and revenue away from CalOptima. And because KP can essentially select the Medi-Cal members it wants, it could leave you with a larger proportion of high-cost patients. What worries you most about the deal? It would have been preferable if the discussion about a direct contract had had more opportunity for input and dialogue versus a kind of surprise announcement. We don’t want a two-tier health system created. Tier one would be, “If you come to Kaiser, we’re going to select who we want to have in our network.” Tier two is everybody else. If it does proceed, we will do everything in our power to make sure it is seamless for the member. Q: What do you think of the state’s new Medi-Cal prescription drug program under Magellan Health? These major statewide initiatives always start off with bumps. There were IT bumps and on the Magellan side some staffing bumps. I think one of the keys was the call wait times, and there was some work that needed to be done with the formulary. But the volume of calls about it from our members is steadily dropping. We still field about 30 calls a day, which is way down. At the height, it was well over 100 a day. It’s smoothing out. Q: There’s a big push in California for greater equity in health care, and Medi-Cal plans are being required to hire chief equity officers. Do you have one? We’re just now finishing a job description, and we will post that position and start looking for candidates. We can actually heat-map where there are disparities and what we suspect to be food insufficiency, unemployment, lack of access to fresh fruits and vegetables. It’s unbelievable the data that’s out there. I want the equity officer to be able to look at that and say strategically, “We’ve got a hole right here. What are we doing here, because we’re missing it?” Q: Let’s talk about CalAIM. Which of its 14 nontraditional services is CalOptima providing at this point? We have started doing housing deposits for CalOptima members who are eligible. We’re also beginning to work on collaborative housing navigation, where we will navigate our members to community support services that get people placed into housing. Another big piece in CalAIM that we are also working on is recuperative care. Q: Can you explain what that is? Recuperative care is pretty basic. It is for individuals who most times are coming from a hospital. They are sometimes homeless or unhoused, and they literally need a place to recuperate. They are not quite ready to go back to a shelter and certainly not back to the streets. While they’re there, staff will work to get them hooked up for housing navigation, job placement, behavioral and mental health services. They have a medical facility on-site so they can see a doctor; they have dentistry to deal with teeth. Q: You seem sharply focused on assisting Orange County’s homeless population. Anybody who’s homeless in Orange County is going to have eligibility for CalOptima because they don’t have resources. I went out on the homeless count in the city of Fountain Valley, and I met face to face with our homeless in their cars, in their vans, in the dirt, in the parks, under the bridges, in their tents, behind buildings, behind dumpsters. And every individual — that’s our member. This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | A Travel Nurse Leaves Fears of Hospital Drug Tampering Across Three States Posted: 14 Apr 2022 02:00 AM PDT Health officials in at least three states are investigating a travel nurse suspected of tampering with and potentially contaminating vials and syringes of opioid painkillers in two hospitals, then returning the vials to medication cabinets where they could be unknowingly given to patients. One hundred patients who may have been exposed to contaminated syringes last year at Johnson City Medical Center in Tennessee were urged to get tested for hepatitis and HIV, according to state documents obtained by KHN through a public records request. The documents also reveal that Raleigh General Hospital in West Virginia this year gave vials to law enforcement to test for evidence of tampering. Those results haven’t been made public. The travel nurse, Jacqueline Brewster, 52, of Belfry, Kentucky, was arrested by her local sheriff’s office on undisclosed charges Tuesday in response to a fugitive warrant from Washington County, Tennessee, where the allegations of tampering began, according to jail and court records. Brewster was released Wednesday with orders to report to Tennessee within 10 days. “I didn’t run away from anything,” Brewster said in court. “I don’t know how I’m a fugitive.” According to documents filed by Tennessee and West Virginia health authorities with their respective nursing boards, Brewster is suspected of repeatedly opening hospital medication cabinets to withdraw vials or syringes of an opioid painkiller, Dilaudid, allegedly removing some of the drug to either use or steal, and then returning the vials or syringes, possibly after gluing a cap back on. The CEO of one of the affected hospital systems alleged in an interview with KHN that the travel nurse added another liquid to syringes — possibly in an attempt to cover her tracks. The allegations against Brewster, which have not been previously reported, come at a time when the coronavirus pandemic forced many U.S. hospitals to rely more than ever on travel nurses, who often cross state lines to work months-long stints in short-staffed hospitals. As the virus flooded hospitals with patients and worsened nursing shortages, many hospitals turned to travel nurses to fill the gaps, often at a dramatically increased cost. But “desperation” to recruit nurses also exacerbated existing flaws in the government infrastructure intended to hold nurses accountable, said John Benson, co-founder of Verisys, a data management company that researches potential employees for health care systems. Nurses and other medical professionals are licensed, investigated, and disciplined at the state level. But investigators don’t communicate well across state lines, Benson said, so as more nurses began to travel during the pandemic, it became easier to “outrun” investigations by getting a new job in another state long before allegations of wrongdoing became public. “The system was broken before covid,” Benson said. “It just got more broken during covid.” Brewster, a registered nurse, has been licensed in Kentucky since 2004 and holds a license permitting her to work in more than 30 states that participate in the Nurse Licensure Compact. After she was accused of tampering at Raleigh General last month, the West Virginia nursing board suspended Brewster’s ability to practice in the state. Days later, Tennessee health officials acted on a complaint they received from Johnson City Medical Center last July, launching a professional disciplinary proceeding that could revoke Brewster’s ability to work in that state later this year. As of Wednesday, Brewster’s multistate license was “under investigation” in Kentucky but otherwise unrestricted, meaning she could still work as a nurse in most of the country. It is unknown where else Brewster might have worked as a travel nurse, including in the seven months after she was first accused of tampering in Tennessee. Brewster could not be reached for comment and it is unclear whether she has an attorney. A Knoxville lawyer listed as Brewster’s attorney in records filed with the Tennessee Board of Nursing denied representing the nurse. One hospital that became heavily dependent on travel nurses during the pandemic was Johnson City Medical Center. Ballad Health, which owns the hospital, said last summer the pandemic increased the number of travel nurses the company employed from about 150 to 400. Brewster was among those hired. She was employed by Jackson Nurse Professionals, a travel nurse company in Orlando, Florida, and worked at the Johnson City Medical Center for three months before the alleged tampering was discovered, according to the records. Ballad Health CEO Alan Levine told KHN another nurse flagged a suspicious vial in the hospital’s medical cabinet, and an internal investigation linked the vial to Brewster. “She was removing the Dilaudid and replacing it with another substance that looked clear like Dilaudid, and replacing the vials in the Omnicell system,” Levine said. “One of our other nurses noticed that something looked different in one of the vials and notified the pharmacy immediately.” Ballad Health fired Brewster and alerted law enforcement and the Tennessee Department of Health, according to a statement from the company. It sent five Dilaudid syringes to the Tennessee Bureau of Investigation’s crime lab, which confirmed the amount of medication within was “inconsistent with the manufacturer’s label,” according to the nursing board documents. The hospital reported that it also tried to give Brewster a drug test. She initially provided an insufficient urine sample, the documents allege, and then after providing a second sample Brewster “accused the lab technician of being corrupt,” grabbed the sample out of his hand, and dumped it down the sink. “This is my *** [sic],” Brewster said as she took back the sample, according to the documents. The Tennessee Department of Health filed the professional disciplinary case against Brewster with the Board of Nursing on March 31. She is scheduled to appear Aug. 24 at a board hearing and risks losing her nursing license. At some point, after she was fired from Johnson City Medical Center, Brewster began to work at Raleigh General, an unrelated hospital about 120 miles to the north in Beckley, West Virginia. Last month, the hospital reported to the West Virginia nursing board that Dilaudid vials in its medicine cabinets appeared to have been tampered with, according to a board order suspending Brewster’s license. Some vials were missing tops and others had tops marked with a residue that “looked like glue,” the board alleges. Once again, an internal investigation “led directly” to Brewster, according to the board order. Raleigh General “disposed of many vials of Dilaudid in order to protect patients from contamination” and provided some vials to law enforcement for testing. Results have not been disclosed. Jackson Nurse Professionals did not respond to requests for comment. It is unclear whether Brewster still works for the company. Raleigh General Hospital in West Virginia released a statement that it was still investigating Brewster and cooperating with authorities but declined to answer questions about the case. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | Persistent Problem: High C-Section Rates Plague the South Posted: 14 Apr 2022 02:00 AM PDT All along, Julia Maeda knew she wanted to have her baby naturally. For her, that meant in a hospital, vaginally, without an epidural for pain relief. This was her first pregnancy. And although she is a nurse, she was working with cancer patients at the time, not with laboring mothers or babies. “I really didn’t know what I was getting into,” said Maeda, now 32. “I didn’t do much preparation.” Her home state of Mississippi has the highest cesarean section rate in the U.S. — nearly 4 in 10 women who give birth there deliver their babies via C-section. Almost two weeks past her due date in 2019, Maeda became one of them after her doctor came to her bedside while she was in labor. “'You’re not in distress, and your baby is not in distress — but we don’t want you to get that way, so we need to think about a C-section,’” she recalled her doctor saying. “I was totally defeated. I just gave in.” C-sections are sometimes necessary and even lifesaving, but public health experts have long contended that too many performed in the U.S. aren’t. They argue it is major surgery accompanied by significant risk and a high price tag. Overall, 31.8% of all births in the U.S. were C-sections in 2020, just a slight tick up from 31.7% the year before, according to the latest data from the Centers for Disease Control and Prevention. But that’s close to the peak in 2009, when it was 32.9%. And the rates are far higher in many states, especially across the South. These high C-section rates have persisted — and in some states, such as Alabama and Kentucky, even grown slightly — despite continual calls to reduce them. And although the pandemic presented new challenges for pregnant women, research suggests that the U.S. C-section rate was unaffected by covid. Instead, obstetricians and other health experts say the high rate is an intractable problem. Some states, such as California and New Jersey, have reduced their rates through a variety of strategies, including sharing C-section data with doctors and hospitals. But change has proved difficult elsewhere, especially in the South and in Texas, where women are generally less healthy heading into their pregnancies and maternal and infant health problems are among the highest in the U.S. “We have to restructure how we think about C-sections,” said Dr. Veronica Gillispie-Bell, an OB-GYN who is medical director of the Louisiana Perinatal Quality Collaborative, a group of 43 birthing hospitals focused on lowering Louisiana’s C-section rate. “It’s a lifesaving technique, but it’s also not without risks.” She said C-sections, like any operation, create scar tissue, including in the uterus, which may complicate future pregnancies or abdominal surgeries. C-sections also typically lead to an extended hospital stay and recovery period and increase the chance of infection. Babies face risks, too. In rare cases, they can be nicked or cut during an incision. Although C-sections are sometimes necessary, public health leaders say these surgeries have been overused in many places. Black women, particularly, are more likely to give birth by C-section than any other racial group in the country. Often, hospitals and even regions have wide, unexplained variations in rates. “If you were delivering in Miami-Dade County, you had a 75% greater chance of having a cesarean than in northern Florida,” said Dr. William Sappenfield, an OB-GYN and epidemiologist at the University of South Florida who has studied the state’s high C-section rate. Some physicians say their rates are driven by mothers who request the procedure, not by doctors. But Dr. Rebekah Gee, an OB-GYN and former secretary of the Louisiana Department of Health, said she saw C-section rates go dramatically up at 4 and 5 p.m. — around the time when doctors tend to want to go home. She led several initiatives to improve birth outcomes in Louisiana, including leveling Medicaid payment rates to hospitals for vaginal deliveries and C-sections. In most places, C-sections are significantly more expensive than vaginal deliveries, making high C-section rates not only a concern for expectant mothers but also for taxpayers. Medicaid pays for 60% of all births in Louisiana, according to KFF, and about half of all births in most Southern states, compared with 42% nationally. That’s one reason some states — including Louisiana, Tennessee, and Minnesota — have tried to tackle high C-section rates by changing how much Medicaid pays for them. But payment reform alone isn’t enough, Gee said. “There was a guy in central Louisiana who was doing more C-sections and early elective deliveries than anyone in the U.S.,” she said. “When you have a culture like that, it’s hard to shift from it.” Linda Schwimmer, president and CEO of the New Jersey Health Care Quality Institute, said many hospitals and doctors don’t even know their C-section rates. Sharing this data with doctors and hospitals — and making it public — made some providers uncomfortable, she said, but it ultimately worked. New Jersey’s C-section rate among first-time, low-risk mothers dropped from 33.1% in 2013 to 26.7% six years later once the state began sharing this data, among other initiatives. The New Jersey Health Care Quality Institute, and other groups like it around the country, focuses on reducing a subset of C-sections called “nulliparous, term, singleton, vertex” C-sections, or surgeries on first-time, full-term moms giving birth to a single infant who is positioned head-down in the uterus. NTSV C-sections are important to track because women who have a C-section during their first pregnancy face a 90% chance of having another in subsequent pregnancies. Across the U.S., the rate for these C-sections was 25.9% in 2020 and 25.6% in 2019. Dr. Elliott Main, a maternal-fetal specialist at Stanford University and the medical director of the California Maternal Quality Care Collaborative, co-authored a paper, published in JAMA last year, that outlines interventions the collaborative took that lowered California’s NTSV C-Section rate from 26.0% in 2014 to 22.8% in 2019. Nationally, the rate was unchanged during that period. Allowing women to labor for longer stretches of time before resorting to surgery is important, he said. The cervix must be 10 centimeters dilated before a woman gives birth. The threshold for “active labor” used to be when the cervix was dilated at least 4 centimeters. In more recent years, though, the onset of active labor has been changed to 5 to 6 centimeters. “People show up at the hospital too early,” said Toni Hill, president of the Mississippi Midwives Alliance. “If you show up to the hospital at 2 to 3 centimeters, you can be at 2 to 3 centimeters for weeks. I don’t even consider that labor.” Too often, she said, women at an early stage of labor end up being induced and deliver via C-section. “It’s almost like, at this point, C-sections are being handed out like lollipops,” said LA’Patricia Washington, a doula based in Jackson, Mississippi. Doulas are trained, nonmedical workers who help parents before, during, and after delivery. Washington works with a nonprofit group, the Jackson Safer Childbirth Experience, that pays for doulas to help expectant mothers in the region. Some state Medicaid programs, such as New Jersey’s, reimburse for services by doulas because research shows they can reduce C-section rates. California has been trying to roll out the same benefit for its Medicaid members. In 2020, when Julia Maeda became pregnant again, she paid out-of-pocket for a doula to attend the birth. The experience of having her son via C-section the previous year had been “emotionally and psychologically traumatic,” Maeda said. She told her OB-GYN that she wanted a VBAC, short for “vaginal birth after cesarean.” But, she said, “he just shook his head and said, 'That’s not a good idea.’” She had VBAC anyway. Maeda credits her doula with making it happen. “Maybe just her presence relayed to the nursing staff that this was something I was serious about,” Maeda said. “They want you to have your baby during business hours. And biology doesn’t work that way.” KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | A Year In, Montana’s Rolled-Back Public Health Powers Leave Some Areas in Limbo Posted: 14 Apr 2022 02:00 AM PDT A year after a new Montana law stripped local health boards of their rulemaking authority, confusion and power struggles are creating a patchwork oversight system that may change how public health is administered long after the pandemic is over. The law, which took effect last April amid criticism of mask mandates and other covid restrictions on businesses, gave local elected leaders the final say in creating public health rules. Supporters said elected officials would be accountable to voters if they abuse that authority, while opponents said the change would inject politics into health decisions. Matt Kelley, CEO of the Montana Public Health Institute, a nonprofit focused on strengthening public health systems, said local health boards still have a duty to protect their communities, but the law limits their power to do so. “Anybody who has ever been in a job where they have a responsibility for something but not the authority to actually get that done knows how hard that is and how bad that feels,” Kelley said. The law was part of a wave of bills passed in statehouses amid a pandemic backlash. At least 26 states adopted laws rolling back public health powers. Montana legislators passed some of the most restrictive changes, including preventing limits on religious gatherings and banning employers — even hospitals — from requiring vaccination against covid-19 or any other disease. Before the new law, health boards comprising appointees by local governments set public health rules and approved emergency health measures for their regions. The measure limiting health boards’ powers allows them to pass orders in an emergency, though the elected officials can change or revoke those orders. Elected officials also have final say in appointing a health officer. But local health departments’ and health boards’ day-to-day operations are supposed to be untouched by the new rules. The law left county commissions to oversee county health boards and city councils to oversee city health boards. But for local governments with joint health departments, the law is vague; they’re left to define their own “governing body” to provide oversight. As a result, those cities and counties have to rework agreements that define how their joint boards operate, said Kelly Lynch, executive director of the Montana League of Cities and Towns. Several haven’t figured it out. In some places, the holdup has been local officials butting heads over who should get a vote and how much sway each should get. In other areas, established bodies have not outlined how they’ll operate. As of early April, four out of six of Montana’s most-populated counties — Missoula, Cascade, Yellowstone, and Gallatin — still hadn’t finalized their governing bodies. That left public health boards in limbo. Many of the health officials stuck in the middle are new to the job after their predecessors quit or retired in the face of an increasingly polarized public. When D’Shane Barnett was hired as health officer for the Missoula City-County Health Department, he expected the new rules to roll into place soon after. A year later, he’s still waiting. “The weirdest impact is that I don’t know who my boss is,” Barnett said. County spokesperson Allison Franz said local officials hope to have a draft interlocal agreement ready for county and city leaders in June. Until then, Barnett said, he tries to make sure all interested local government officials are on board with his department’s actions. “So far, everybody is, but it won’t be that way forever,” he said. David Bedey, a Republican state representative from Ravalli County who proposed the new law last year, said the idea to shift public health authority to elected officials preceded the pandemic. Although politicians aren’t experts in roadways, they craft the rules of the road — and the same idea should apply to public health, he said. Bedey said he’s surprised it’s taken localities this long to establish governing bodies, but he believes they’ll work it out. “The idea here was local jurisdictions and citizens within those jurisdictions would settle this amongst themselves,” Bedey said. “If they have pending regulations that need approval, that ought to give them plenty of motivation.” John Felton, Yellowstone County’s health officer, said the law has created confusion in the state’s largest county. There, four jurisdictions — the county, the cities of Billings and Laurel, and the town of Broadview — overlap in oversight of a health department, RiverStone Health, which has its own clinics and offers medical services beyond the scope of most public health agencies in the state. Felton wonders how new oversight might affect future changes in non-covid areas of public health, such as food prep rules or how tattoo artists wrap clients’ new ink. He’s waiting to see how local leaders define a governing body’s interactions with other new laws, such as one that restricts health officials from getting between a business and its clients. But with covid cases low, those once-pressing questions seem to have fizzled out. “Without that urgency and concern that someone’s going to put in masking requirements or occupancy limitations, it kind of gets forgotten,” Felton said. Even with the uncertainty, Felton said, he’ll act if a public health issue puts people at risk: “I will just do what I believe is the right thing and sort it out later if someone doesn’t like the way it was, or they think it was contrary to the intent of the rules.” In the law, the authors wrote that part of its purpose was to address issues or conditions created during a public health emergency, not to hinder the non-emergency powers of local health boards. Gallatin County Commissioner Joe Skinner, a supporter of the change, said restaurant inspections, septic permits, and the like should be left to health professionals. “When you start restricting people’s freedoms, closing businesses, requiring certain things like masks, that’s not a health decision anymore,” he said. “That’s a political decision that should be made by people that are elected.” For months, Skinner and his fellow county commissioners wanted to be the sole representatives on the new public health authority governing board over the Gallatin City-County Health Department. City leaders from Bozeman and Belgrade objected to being shut out. County officials signed on to a proposal allowing a representative from each city, but some public health workers — including Kelley, a former Gallatin City-County health officer — objected that the plan goes beyond the law by requiring the county’s approval of the health board’s spending. Bozeman Mayor Cyndy Andrus said city officials were reviewing the latest proposal. “The legislature may have made a long-term decision based on what I would call a short-term event,” she said. “You know, 99% of what public health boards do is not pandemic-related.” In Missoula, Barnett said it will take time to understand all the consequences of the law. “This has added a layer of bureaucracy, and it brings popular opinion into public health,” he said. “There are probably going to be effects and ramifications from this bill that we might not see for years.” KHN reporter Jacob Owens contributed to this story. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | When Symptoms Linger for Weeks, Is It Long Covid? Posted: 13 Apr 2022 02:00 AM PDT Many Americans are discovering that recovering from covid-19 may take weeks or even months longer than expected, leaving them with lingering symptoms like intense fatigue or a racing pulse. But does that mean they have what’s known as long covid? Though such cases may not always amount to debilitating long covid, which can leave people bedridden or unable to perform daily functions, it is common to take weeks to fully recover. “There could be more to help people understand that it’s not always a quick bounce back right away after the initial infection,” said Dr. Ben Abramoff, director of the Post-COVID Assessment and Recovery Clinic at Penn Medicine in Philadelphia. “This is still a very significant viral infection, and sometimes it’s just a more gradual recovery process than people’s previous viral illnesses.“ Recent federal health guidelines — which recommend only five days of isolation for those who test positive and are symptom-free — may inadvertently suggest most recoveries are, if not just five days long, pretty quick. That’s the message I got, at least. I’ve reported on the coronavirus pandemic since it started, and I thought I knew what an infection would be like for a young, otherwise healthy person like me. I knew even mild cases could develop into long covid. I thought they were relatively rare. Like many Americans, I found myself slowed by a recovery that took more than a month — far longer than I had expected. I got covid over Christmas. I was vaccinated and boosted, and my symptoms were mild: sore throat, sinus pressure and headache, extreme fatigue. I felt better after eight days, and I tested negative two days in a row on a rapid antigen test. Soon after ending isolation, I had dinner with a friend. One glass of wine left me feeling like I’d had a whole bottle. I was bone-achingly exhausted but couldn’t sleep. The insomnia continued for weeks. Activities that once energized me — walking in the cold, riding an exercise bike, taking a sauna — instead left me intensely tired. The waves of fatigue, which I started calling “crashes,” felt like coming down with an illness in real time: weakened muscles, aches, the feeling that all you can do is lie down. The crashes would last a couple of days, and the cycle would repeat when I accidentally pushed myself beyond my new, unfamiliar limit. My colleague Kenny Cooper is also young, healthy, vaccinated, and boosted. He was sick for almost two weeks before testing negative. His symptoms lingered a few more weeks. A persistent cough kept him from leaving the house. “I just felt like there were weights on my chest. I couldn’t sleep properly. When I woke up, if I moved around too much, I would start coughing immediately,” he said. Abramoff has seen about 1,100 patients since Penn’s post-covid clinic opened in June 2020. There is no official threshold at which someone officially becomes a long-covid patient, he said. The clinic takes a comprehensive approach to patients who have had symptoms for months, evaluating and referring them to specialists, like pulmonologists, or social workers who can assist with medical leave and disability benefits. Those coming to the clinic with symptoms lasting six to eight weeks, Abramoff said, are generally sent home to rest. They will likely get better on their own. He advises patients with lingering symptoms to adopt a “watchful waiting” approach: Keep in contact with a primary care doctor, and take things slowly while recovering. “You have got to build based on your tolerance,” he said. “People were very sick, even if they weren’t in the hospital.” A National Institutes of Health-funded study on long covid, called Recover, designates any case with symptoms lasting more than 30 days as long covid. Dr. Stuart Katz, a New York University cardiologist who is the study’s principal investigator, said he estimates 25% to 30% of the nearly 60,000 covid patients in the study will fit the long-covid criteria. The 30-day mark is an arbitrary cutoff, Katz said. “There’s this whole spectrum of changing symptoms over time.” A study published in Nature last year tracked more than 4,000 covid patients from initial infection until symptoms subsided. Roughly 13% reported symptoms lasting more than 28 days. That dropped to 4.5% after eight weeks and 2.3% after 12 weeks, indicating most people with symptoms lasting more than a month will recover within another month or two. That leaves potentially millions of Americans suffering from a variety of covid symptoms — some debilitating — and a lingering burden on the health care system and workforce. Recent research from the Brookings Institution estimated that lasting covid symptoms could be responsible for up to 15% of the unfilled jobs in the U.S. labor market. It took me about six weeks to start feeling better. My crashes got better, slowly, as a result of diligent rest and almost nothing else. My colleague, Cooper, has also improved. His coughing fits have subsided, but he’s still dealing with brain fog. The way most studies to date describe long covid would leave us out. But what I’ve come to think of as my “medium covid” affected my life. I couldn’t socialize much, drink, or stay up past 9:30 p.m. It took me 10 weeks to go for my first run — I’d been too afraid to try, fearing another crash that would set me back again. Failing to treat covid as a serious condition could prolong recovery. Patients should monitor and care for themselves attentively, no matter how mild the infection may seem, Abramoff said. “It’s something that could kill somebody who’s in their 70s,” he said. “It’s not nothing.” This story is part of a partnership that includes WHYY, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | Private Equity Ownership of Nursing Homes Triggers Capitol Hill Questions — And a GAO Probe Posted: 13 Apr 2022 02:00 AM PDT In his State of the Union address last month, President Joe Biden focused attention on how private equity ownership of nursing homes can affect residents’ health. “As Wall Street firms take over more nursing homes, quality in those homes has gone down and costs have gone up. That ends on my watch,” Biden said. Those comments dovetail with growing interest from Congress. The Government Accountability Office, for instance, is investigating the ownership of nursing homes, including by private equity firms, and expects to issue a report in the fall, said Chuck Young, the GAO’s managing director of public affairs. “The full scope of what we will cover has not been set yet, however the work will likely be focused on the information [the Centers for Medicare & Medicaid Services] has about nursing home ownership and how the agency uses that information,” Young wrote in an email. The investigation comes in response to a pre-pandemic request from House Ways and Means Committee Chairman Richard Neal (D-Mass.). Yet the pandemic has also underscored the importance of oversight of nursing homes, in light of the lives lost to covid-19. Rep. Bill Pascrell (D-N.J.) submitted a second request to the GAO in 2021 regarding private equity investments in health care. It’s in GAO’s queue, but work on it hasn’t started, Young said. The exponential growth in these private equity investments in recent years “has been associated with a host of trends that are negatively impacting the American people” — including an increase in nursing home mortality rates, wrote Pascrell, who chairs the Ways and Means Oversight Subcommittee. He noted the need to “better understand” the consequences of private equity’s involvement in health care and “the far-reaching impact” of “bankruptcies or closures following PE buyouts.” Pascrell said in a statement to KHN that the data the GAO could compile would be valuable in assessing the reach and impact of such investments: “It is my hope GAO will shed more light and provide more information on Wall Street’s dangerous growing control over nursing homes and long-term care facilities.” That Neal and Pascrell had to ask the GAO for information underscores the dearth of data on nursing home ownership. A June 2021 report by the Medicare Payment Advisory Commission found that information about the effect of private equity ownership on nursing home finances and quality of care was dated and the results of studies were mixed. Democratic House staffers told KHN that because private equity has stepped up its interest in this industry, it’s even more crucial to understand how residents’ health outcomes and staff working conditions compare with those in facilities not owned by private equity companies. From 2010 to 2019, there was a large increase in private equity companies buying up nursing homes, along with other investments in health care. An exact figure is elusive because private purchases are difficult to track, but it’s estimated that such groups own anywhere from 5% to 11% of nursing homes nationwide. A growing body of research shows that health outcomes in private equity-owned facilities are worse than in those under other ownership. A February 2021 study from the National Bureau of Economic Research found that going to a facility owned by a private equity firm increased the chance that a resident would die by 10%, compared with living in another type of facility. That study was conducted from 2005 to 2017. A November 2021 Cornell University study found that residents of private equity-owned nursing homes were more likely to have emergency room visits or be hospitalized than residents of other for-profit homes. Both studies found that Medicare’s costs per resident were higher, meaning more taxpayer dollars were being spent in private equity facilities. Industry trade associations dismissed these findings, saying the studies don’t show the whole picture of how care at private equity-owned homes might differ from that at other facilities. “The focus on private equity ownership of nursing homes is a red herring,” said Mark Parkinson, president and CEO of the industry group the American Health Care Association/National Center for Assisted Living. In his statement, he added that these investor groups have moved on to other, “more lucrative” health care sectors. There is evidence that private equity is increasing investments in home health care and hospices, as more older Americans choose to age in place. “If policymakers want to talk about private equity, then this is a conversation for the entire health care system, not just nursing homes,” Parkinson said. The American Investment Council, an advocacy group for the private equity industry, countered these research findings with other studies. One showed that private equity-owned nursing homes fared better under covid, and another found that living in private equity-backed homes didn’t affect residents’ quality of care (though this study used old data and had a limited sample size). Still, it’s undisputed that private equity firms are buying nursing homes because they’re likely to be profitable, said Robert Tyler Braun, an assistant professor of population health sciences at Cornell University who was an author of the November 2021 study. “The main appealing thing is the margins are low and they’re getting valuable real estate with the purchase,” Braun said. “Plus, the way these deals are structured, it allows you to bring in parties that private equity firms might own, such as maid services [and] clinician services,” and charge higher rates than the market indicates. Profits can also be maximized by reducing staff levels or hours, affecting residents’ care, said Eileen O’Grady, research and campaign manager for the Private Equity Stakeholder Project, a private equity watchdog group. The Biden administration is trying to improve nursing home quality — for example, by directing Medicare to set higher standards for the facilities and instructing the Department of Health and Human Services to examine private equity ownership. But some initiatives will require the assistance of Congress, which so far has been slow to move on oversight. Efforts have remained in the data-gathering phase. The last GAO report about private equity ownership of nursing homes, released in 2011 — more than 10 years ago — found some differences in care and financial performance between for-profit facilities and those with nonprofit ownership. Meanwhile, the National Academies of Sciences, Engineering, and Medicine has released a much-publicized 600-page report calling for more data transparency on nursing home performance and finances to understand how ownership affects care, among other recommendations for improving the nursing home system overall. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | | Who Doesn’t Text in 2022? Most State Medicaid Programs Posted: 13 Apr 2022 02:00 AM PDT West Virginia will use the U.S. Postal Service and an online account this summer to connect with Medicaid enrollees about the expected end of the covid public health emergency, which will put many recipients at risk of losing their coverage. What West Virginia won’t do is use a form of communication that’s ubiquitous worldwide: text messaging. “West Virginia isn’t set up to text its members,” Allison Adler, the state’s Medicaid spokesperson, wrote to KHN in an email. Indeed, most states’ Medicaid programs won’t text enrollees despite the urgency to reach them about renewing their coverage. A KFF report published in March found just 11 states said they would use texting to alert Medicaid recipients about the end of the covid public health emergency. In contrast, 33 states plan to use snail mail and at least 20 will reach out with individual or automated phone calls. “It doesn’t make any sense when texting is how most people communicate today,” said Kinda Serafi, a partner with the consulting firm Manatt Health. State Medicaid agencies for months have been preparing for the end of the public health emergency. As part of a covid relief law approved in March 2020, Congress prohibited states from dropping anyone from Medicaid coverage unless they moved out of state during the public health emergency. When the emergency ends, state Medicaid officials must reevaluate each enrollee’s eligibility. Millions of people could lose their coverage if they earn too much or fail to provide the information needed to verify income or residency. As of November, about 86 million people were enrolled in Medicaid, according to the Centers for Medicare & Medicaid Services. That’s up from 71 million in February 2020, before covid began to ravage the nation. West Virginia has more than 600,000 Medicaid enrollees. Adler said about 100,000 of them could lose their eligibility at the end of the public health emergency because either the state has determined they’re ineligible or they’ve failed to respond to requests that they update their income information. “It’s frustrating that texting is a means to meet people where they are and that this has not been picked up more by states,” said Jennifer Wagner, director of Medicaid eligibility and enrollment for the Center on Budget and Policy Priorities, a Washington-based research group. The problem with relying on the Postal Service is that a letter can get hidden in “junk” mail or can fail to reach people who have moved or are homeless, Serafi said. And email, if people have an account, can end up in spam folders, she noted. In contrast, surveys show lower-income Americans are just as likely to have smartphones and cellphones as the general population. And most people regularly use texting. In Michigan, Medicaid officials started using text messaging to communicate with enrollees in 2020 after building a system with the help of federal covid relief funding. They said texting is an economical way to reach enrollees. “It costs us 2 cents per text message, which is incredibly cheap,” said Steph White, an enrollment coordinator for the Michigan Department of Health and Human Services. “It’s a great return on investment.” CMS officials have told states they should consider texting, along with other communication methods, when trying to reach enrollees when the public health emergency ends. But many states don’t have the technology or information about enrollees to do it. Efforts to add texting also face legal barriers, including a federal law that bars texting people without their consent. The Federal Communications Commission ruled in 2021 that state agencies are exempt from the law, but whether counties that handle Medicaid duties for some states and Medicaid managed-care organizations that work in more than 40 states are exempt as well is unclear, said Matt Salo, executive director of the National Association of Medicaid Directors. CMS spokesperson Beth Lynk said the agency is trying to figure out how Medicaid agencies, counties, and health plans can text enrollees within the constraints of federal law. Several states told KHN that Medicaid health plans will be helping connect with enrollees and that they expect the plans to use text messaging. But the requirement to get consent from enrollees before texting could limit that effort. That’s the situation in Virginia, where only about 30,000 Medicaid enrollees — out of more than a million — have agreed to receive text messages directly from the state, said spokesperson Christina Nuckols. In an effort to boost that number, the state plans to ask enrollees if they want to opt out of receiving text messages, rather than ask them to opt in, she said. This way enrollees would contact the state only if they don’t want to be texted. The state is reviewing its legal options to make that happen, she said. Meanwhile, Nuckols added, the state expects Medicaid health plans to contact enrollees about updating their contact information. Four of Virginia’s six Medicaid plans, which serve the bulk of the state’s enrollees, have permission to text about 316,000, she said. Craig Kennedy, CEO of Medicaid Health Plans of America, a trade group, said that most plans are using texting and that Medicaid officials will use multiple strategies to connect with enrollees. “I do not see this as a detriment, that states are not texting information about reenrollment,” he said. “I know we will be helping with that.” California officials in March directed Medicaid health plans to use a variety of communication methods, including texting, to ensure that members can retain coverage if they remain eligible. The officials told health plans they could ask for consent through an initial text. California officials say they also plan to ask enrollees for consent to be texted on the enrollment application, although federal approval for the change is not expected until the fall. A few state Medicaid programs have experimented in recent years with pilot programs that included texting enrollees. In 2019, Louisiana worked with the nonprofit group Code for America to send text messages that reminded people about renewing coverage and providing income information for verification. Compared with traditional communication methods, the texts led to a 67% increase in enrollees being renewed for coverage and a 56% increase in enrollees verifying their income in response to inquiries, said Medicaid spokesperson Alyson Neel. Nonetheless, the state isn’t planning to text Medicaid enrollees about the end of the public health emergency because it hasn’t set up a system for that. “Medicaid has not yet been able to implement a text messaging system of its own due to other agency priorities,” Neel said. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation. USE OUR CONTENTThis story can be republished for free (details). | |
































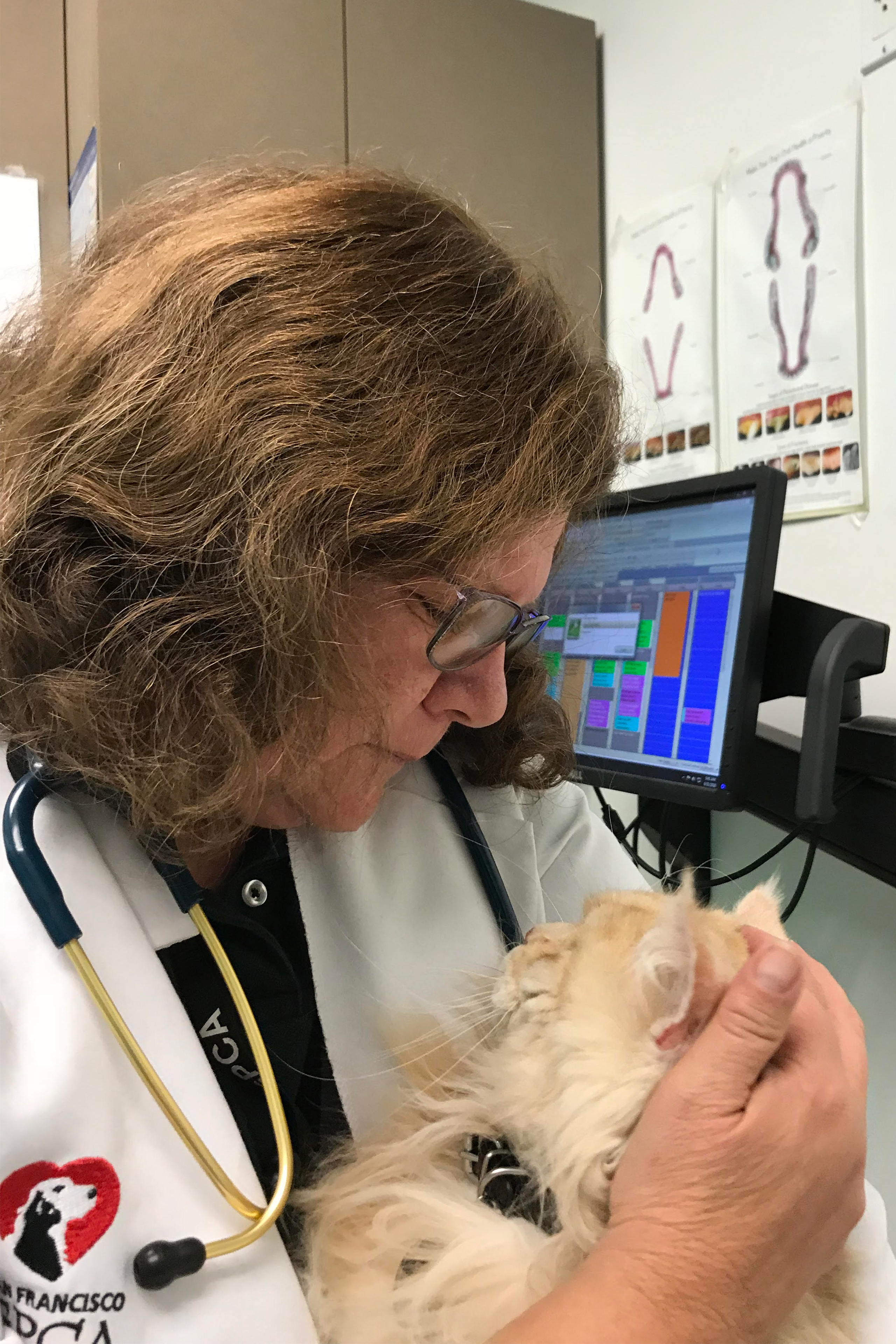


No comments:
Post a Comment